If you want a simple answer to “how is a dental implant done”: a titanium or zirconia post is placed into the jawbone, allowed to fuse with bone, and then topped with an abutment and crown to replace a missing tooth. This guide walks you step-by-step through what to expect from the first consult to the final crown, including tests, surgery, healing, risks, and how to prepare — with specifics useful for those asking how is a dental implant done in Aurora, IL.
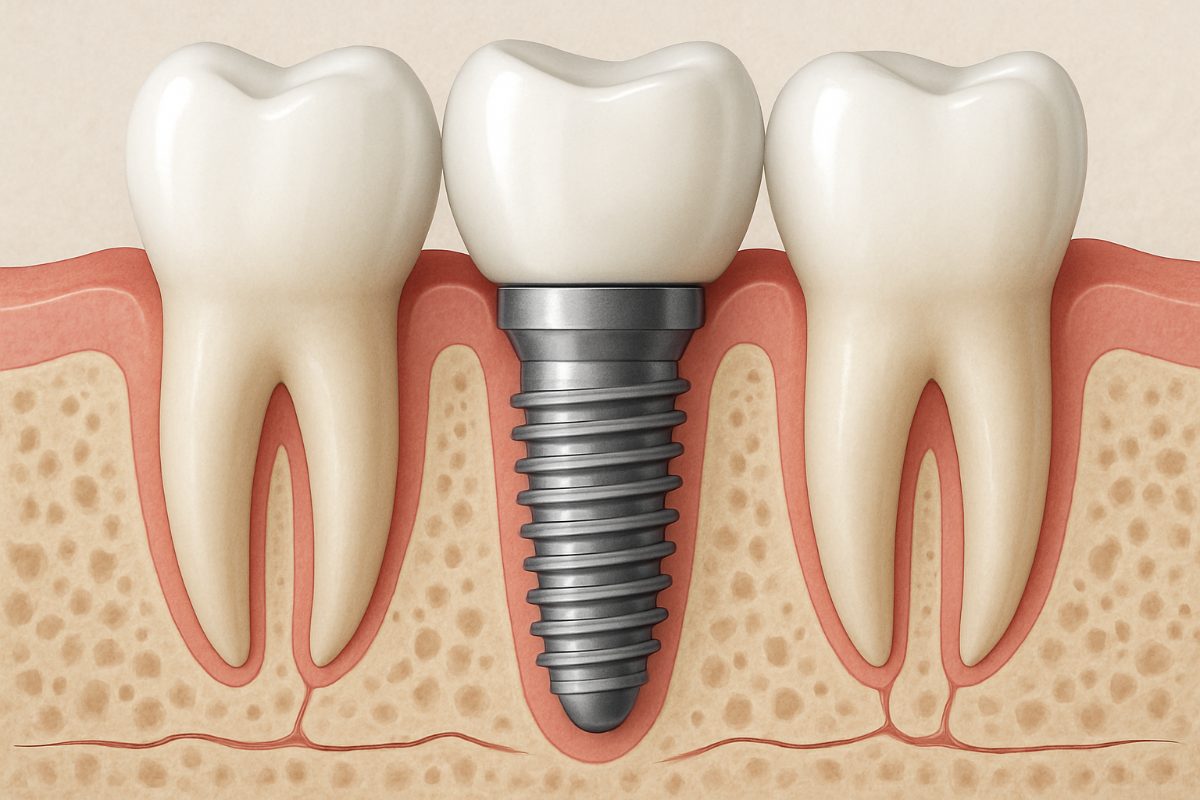
What is a dental implant?
A dental implant is a small post, usually titanium or zirconia, that acts like a tooth root. The implant is placed in the jawbone. An abutment connects the implant to a crown, bridge, or denture. The crown is the visible tooth replacement made from materials like porcelain or zirconia. Together, implant + abutment + crown replace both the root and the visible tooth for long-term function and appearance.
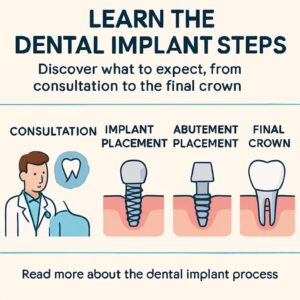
Quick overview: how is a dental implant done — the big picture
The process has five main phases: consultation and diagnostics, treatment planning and any prep work, implant placement surgery, healing and osseointegration, and the final restoration. If you’re wondering how is a dental implant done in Aurora, IL, expect the entire timeline to range from a few months to a year depending on extra treatments and healing needs.
Step 1: Initial consultation and diagnostics
Medical and dental history
Your dentist will ask about health conditions, medications, smoking, and past dental problems. Conditions like uncontrolled diabetes, certain medications, or heavy smoking can affect healing and implant success. Honest answers help the team choose the safest plan.
Exams and imaging
Expect a clinical exam plus imaging. A CBCT 3D scan shows bone volume, nerve positions, and sinus anatomy. Intraoral scans capture your bite and tooth shapes. These images are key to answering “how is a dental implant done” with precision and lowering surgical risk.
Step 2: Treatment planning and preparation
Digital treatment planning
Computer-guided planning places the virtual implant in the exact position for best function and looks. The plan maps the implant relative to bone and nearby nerves and shows the final tooth shape. Guided surgery templates or navigation tools let the surgeon follow that plan during placement.
Preparatory treatments
Some patients need tooth extractions, bone grafts, or gum procedures before implant placement. Bone grafts build up the jaw when bone has shrunk after tooth loss. These steps add healing time but create the stable foundation implants need.
Step 3: Implant placement surgery
Anesthesia and sedation choices
Local anesthesia is standard. Nitrous oxide (laughing gas) and oral or IV sedation are options for comfort and anxiety. Your medical history and procedure complexity help decide the best choice. You can typically expect to be relaxed and comfortable throughout.
The surgical steps
The surgeon exposes the bone, drills a small site, and places the implant post. The site is closed with sutures or a healing cap. Immediate post-op notes include mild swelling and soreness that peak in 48–72 hours and fade with proper care.
Step 4: Healing and osseointegration
Bone typically fuses to the implant in 3–6 months — this is osseointegration. Good oral hygiene, avoiding smoking, and following dietary guidance support success. Signs of normal healing include reduced swelling, minimal pain, and stable tissues around the implant.
Interim restorations and follow-up visits
Temporary crowns or removable prosthetics can be used during healing for aesthetics and function. Regular follow-ups check integration and soft-tissue health. Your team will advise a schedule of visits to monitor progress.
Step 5: Final restoration — abutment and crown
Once healed, the abutment is attached to the implant and impressions or digital scans are taken for the final crown. The lab then fabricates the crown, which is secured to the abut. Final adjustments ensure correct bite, comfort, and appearance.
Zirconia and other restorative materials
Zirconia crowns are strong, stain-resistant, and highly esthetic. Other materials include porcelain-fused-to-metal and ceramic options. In-house labs and digital workflows often deliver more accurate fits and faster turnaround.
Common risks and how they’re managed
Risks include infection, implant failure, nerve irritation, and sinus involvement for upper implants. Most issues are preventable or treatable: infections respond to antibiotics and cleaning, failed implants can be removed and replaced after healing, and careful planning with CBCT reduces nerve or sinus risks.
How modern tech lowers risk
CBCT scans, guided surgery, soft-tissue lasers, and digital workflows improve accuracy, reduce surprises, and speed treatment. These tools lower the chance of complications and improve long-term outcomes.
How to prepare and what to expect the day of surgery
Follow pre-op instructions: avoid eating if sedated, arrange a ride home, and wear comfortable, loose clothing. Expect mild swelling and tenderness afterward. Rest, ice, and prescribed pain meds or over-the-counter options help control discomfort.
Post-op care tips
Use prescribed antibiotics or mouth rinse as directed. Stick to a soft diet for a few days, avoid smoking, and keep the area clean with gentle brushing. Contact your office for heavy bleeding, severe pain, fever, or numbness lasting beyond a day or two. More Post-op care tips are available.
Cost, insurance, and financing basics
Costs vary by implant type, number of implants, preparatory work, and materials. Dental insurance may cover part of the restorative crown but often limits implant coverage. Many practices offer financing, third-party plans, or in-house payment options to spread costs.
Why choose Grand Dental Implant Centers for dental implants
Grand Dental Implant Centers offers implant-focused care across Illinois, with CBCT imaging, in-house labs, zirconia restorations, IV sedation, and full-mouth solutions. Experienced implant clinicians lead care at locations like Aurora, so patients get a streamlined, start-to-finish approach backed by modern tech and compassionate service.
Questions to ask your implant dentist
Ask about the dentist’s implant experience and complication rate, what materials they use, sedation options, the expected timeline, costs, and warranty or aftercare policies. Clear answers help you feel confident about the plan.
Conclusion and next steps
In short, when people ask “how is a dental implant done” they’re asking about a staged process of planning, placement, healing, and restoration that replaces a tooth root and crown. If you’re considering implants and want care that uses CBCT, digital planning, and experienced clinicians, schedule a consultation with Grand Dental Implant Centers to review your options and timeline.